It is estimated that 80% of the UK population will at some point in their lives require treatment for spinal pain and 5% will develop long-term pain, requiring a spinal implant in many cases.
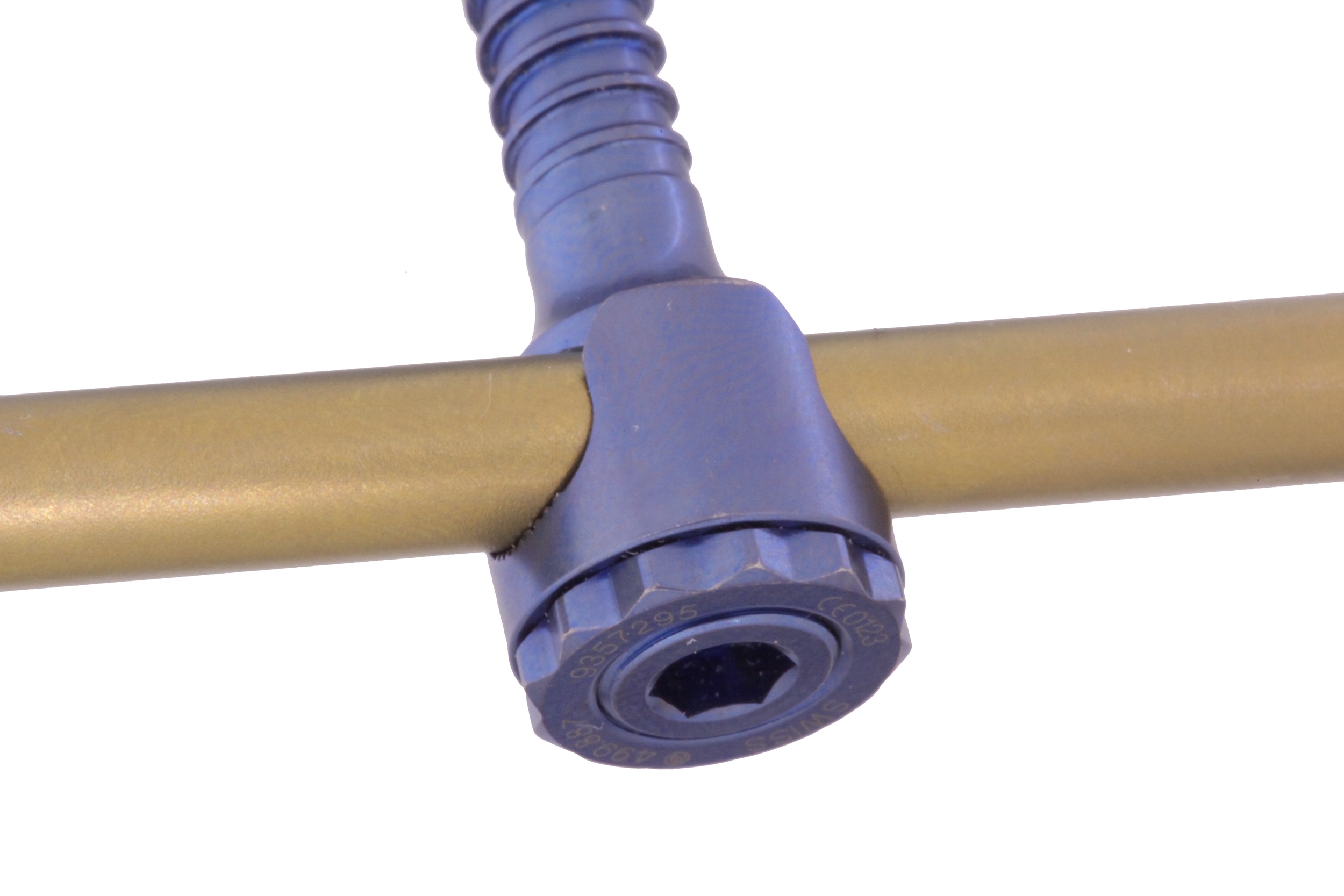
The clinical success of these implants is affected by (1) surgical technique, (2) implant design and material, and (3) the individual patient. Although advances in spinal instrumentation have enabled greater correction of spinal deformities and increased fusion rates, instrumentation failure continue to be problematic and remain poorly understood. Reported problems include corrosion, pseudoarthrosis, implant debris-induced osteolysis, granuloma formation due to inflammatory reaction secondary to fretting corrosion of the implant. Recent research suggests a dramatic rise in early failure of spine implants that contain junctions between two metal parts (i.e. modular), such as titanium and cobalt-chromium. The cause is most likely corrosion that releases metal into the body, resulting in inflammatory reactions severe enough to destroy muscle, tendon and ligaments and to create masses capable of compressing nerves and veins.
Extensive retrieval analysis of failed hip replacement components at our centre has revealed that corrosion of the implant plays a significant role in failure. A number of clinical studies have also reported visual evidence of corrosion of spinal implants during revision surgery. It is speculated that this corrosion process is responsible for the release of metal debris, leading to the destruction of soft tissue and the formation of solid masses. However the modes and mechanisms of corrosive damage of spinal implants and the factors that effect it are unclear.
The LIRC has received funding from K2M to conduct research on retrieved spinal implants and associated clinical data to improve understanding of spine implant failure, surgical technique and implant design to create long lasting spine implants.